Kids Hurt More Than They Have to and That Is Dumb
How the drive to solve a solvable problem led to the creation of the Meg Foundation. Read our story.
Jody Thomas, PhD
Babies & Toddlers (0-2) Kids (3-11) Tweens & Teens (12+) Needle Pokes Provider Acute Pain Chronic Pain Procedural Pain English Pain Management
Share this:
Solving a Solvable Problem by Creating the Meg Foundation

When you nearly die in a horrific car accident at just 17 years old, it tends to change how you see the world. It certainly did for me. Looking back with the advantage of over two and half decades of perspective since that fateful day, I realize now that it also set me squarely on the path that lead me to found the Meg Foundation.
A long and painful recovery motivated me to start volunteering on the pediatric oncology unit as a likely annoyingly eager Stanford freshman a year and a half after that accident. I spent countless hours playing games, doing art projects, and entertaining kids while they went through chemo infusions and endured long hours of cancer treatment.
For anyone who ever WAS a kid, let alone has one of their own, it’s not hard to imagine that despite all the scary unknowns of having a disease like cancer, often the most upsetting things for these kids day to day was the pain they experienced being poked and prodded. It was often traumatic. And I mean traumatic in the literal, speaking-as-a-psychologist, sense of the word.
By the time I started my official graduate school training experience to be a pediatric health psychologist at 23 years old, I was already intimately familiar with the heartbreaking suffering medically compromised kids endure through the countless procedures and needles and medical tests.
What I wasn’t prepared for, however, was learning this: a lot of that suffering can be avoided. There are really good procedural pain management methods out there. And it isn’t that hard. And it isn’t expensive. And there are years of research that demonstrate why and how well they work. So much research, in fact, that major medical organizations like the World Health Organization and American Academy of Pediatrics say they are best practice guidelines and should be standard of care. They just weren’t used. Very few providers actually follow these guidelines.
My first reaction: shock. Wait…what? How could this be? How could all these kids, families, and medical providers not know this?
Then came the second reaction: upset. If I’m honest, anger. Why are these kids hurting when they don’t need to be? How can we be failing them so badly? How could we unintentionally but unquestionably be causing so much negative impact, both immediate and long term?
And then, well, I became a little obsessed. Some might say a lot obsessed. Pain became my thing, as they say. I trained hard. I found mentors in the field. I went to conferences, read articles, dove into the research, did some of my own research studies, made sure my clinical training placements put me in the position to learn even more. I joined forces with and learned from the thankfully very many people in my professional world who share this passion. And I worked hard at finding new and better ways to pass that important information along to the families I was lucky enough to work with, and was fortunate enough to see what a positive impact it made on their experience.
I made sure the kids and families I worked with not only knew the pain management tools, but also how to effectively ask for them, and in some cases, demand them.
My decades of experience both as a medical professional and as a patient with a chronic illness made it clear advocacy was a very necessary and even essential skill. Why? The healthcare system as it stands is full of amazing providers. Truly incredible souls that I have come to respect and appreciate in ways I’m not sure I can capture in words. However, that system is still a system that more often than not fails to do what it should when it comes to kids and pain. So, one of the most important skills I ever teach is how to work within that flawed system to get what parents and caregivers need for their child and themselves.
My frustration about this process was always, “how can we reach more people?” How can we make sure that everyone has access to what I (and so many providers like me) can teach families? And it was in this frustration that the Meg Foundation was born. After all, I went to Stanford. I lived for years in the Silicon Valley. I came back to Stanford as faculty at the med school. I was practically marinating in the excitement and possibilities of technology and good design that were happening all around me.
And the vision emerged: bring the worlds of tech and pain work together to create the access for kids and families that I’d been dreaming about for years. Within this model, we could go directly to the people who were most invested, and EMPOWER THEM.
When I train medical providers, one of the first things I like to do is ask them to close their eyes and think of their earliest memory. For a very large majority, their first memory is like mine: a traumatic medical one. For me, it was being held down by several strangers to get a blood test when I was four years old. I was terrified. I was hurting. Forty years later, when I close my eyes and think about it, I can still see the Muppets poster that was on the wall as I screamed hysterically for my mother, who was listening helplessly from the waiting room. It defined how I felt about going to the doctor for years.
So when I ask these clinicians to open their eyes, I remind them how we can teach them some simple techniques and strategies to make sure their own patients don’t have a memory of them like that. That they can give their patients the gift of comfort and safety.
And now, the Meg Foundation is dedicated to giving that same gift to you: the skills, support and tools you need to make sure your child’s first memories aren’t bad medical ones. To make sure they know it doesn’t have to hurt. To show them that they can have control over their experience. To make sure we set them up for a lifetime of good health care experiences right from the start. It’s possible. It’s very, very possible. And we are working hard every day to make it easier and easier to make that a reality for each and every child and family out there.
To learn more about how powerful and how simple good pain management can be, visit our resources.
And please don’t hesitate to reach out to share your pain story, ask a question or suggest a topic you think we should cover. We really want to hear from you. We need you to help us figure out the best path forward to transform the way the world thinks about kids and pain!
You can always reach us at info@megfoundationforpain.org or fill out the form below!
You May Also Be Interested In

Video
Breathing for Comfort with SuperMeg!
Deep breathing is the ultimate hack of your nervous system. Discover how it can help you feel more calm and comfortable by letting Super Meg guide you to find that pace that is right for you.
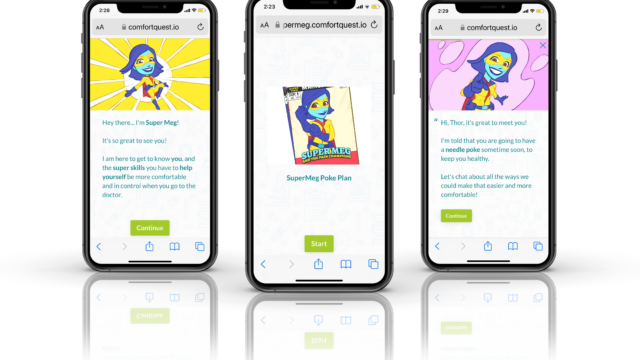
Digital Tool
SuperMeg Poke Planner
Have no fear, SuperMeg is here! This interactive tech helps your child create a plan for being more calm and comfortable during needle pokes.
Video
Built to Empower: Pain Management Tools for All
Dr. Jody Thomas talks about how the Meg Foundation's freely available resources and tools are designed to empower kids, families, and adults to better manage their pain experience.

About the Author
Dr. Jody Thomas is a licensed clinical psychologist, and specialist in pediatric medical illness and trauma. A well-known expert in pediatric pain who teaches internationally on the subject, she is also a founder and the former Clinical Director of the Packard Pediatric Pain Rehabilitation Center at Stanford, and a former Assistant Professor at the Stanford University School of Medicine. Though she now lives in Denver, CO, she still serves as Adjunct Faculty for Stanford, providing supervision and teaching. As a consultant for the Lucile Packard Children’s Hospital at Stanford, she directs projects on the integration and innovation of pain management using tech-based intervention. Her passion for bringing together the power of medical science, technology and design to transform the way we think about kids and pain led her to her current focus but it’s her role as a mom of two that solidified her path in creating the Meg Foundation.