Can holding children down for shots traumatize them? A health psychologist says yes.
While science and best practice guidelines from top medical organizations clearly say holding down kids is a very bad idea, it still happens every single day.

Jody Thomas, PhD
Babies & Toddlers (0-2) Kids (3-11) Tweens & Teens (12+) Needle Pokes Provider Procedural Pain English
Share this:
I’m a health psychologist and expert in medical illness, trauma, and pain with 25 years of experience in health care settings. If I could wipe out any practice that happens on the daily in medicine, VERY high on my list is holding down kids for medical procedures. While science and best practice guidelines from top medical organizations clearly say holding down kids is a terrible idea and can cause medical trauma, it still happens every single day. To be blunt, holding a child down for a shot or needle stick is wrong and can cause lifelong damage to their relationship with healthcare providers.
— Point of View Comic —
A Childhood memory: Being held down for a shot
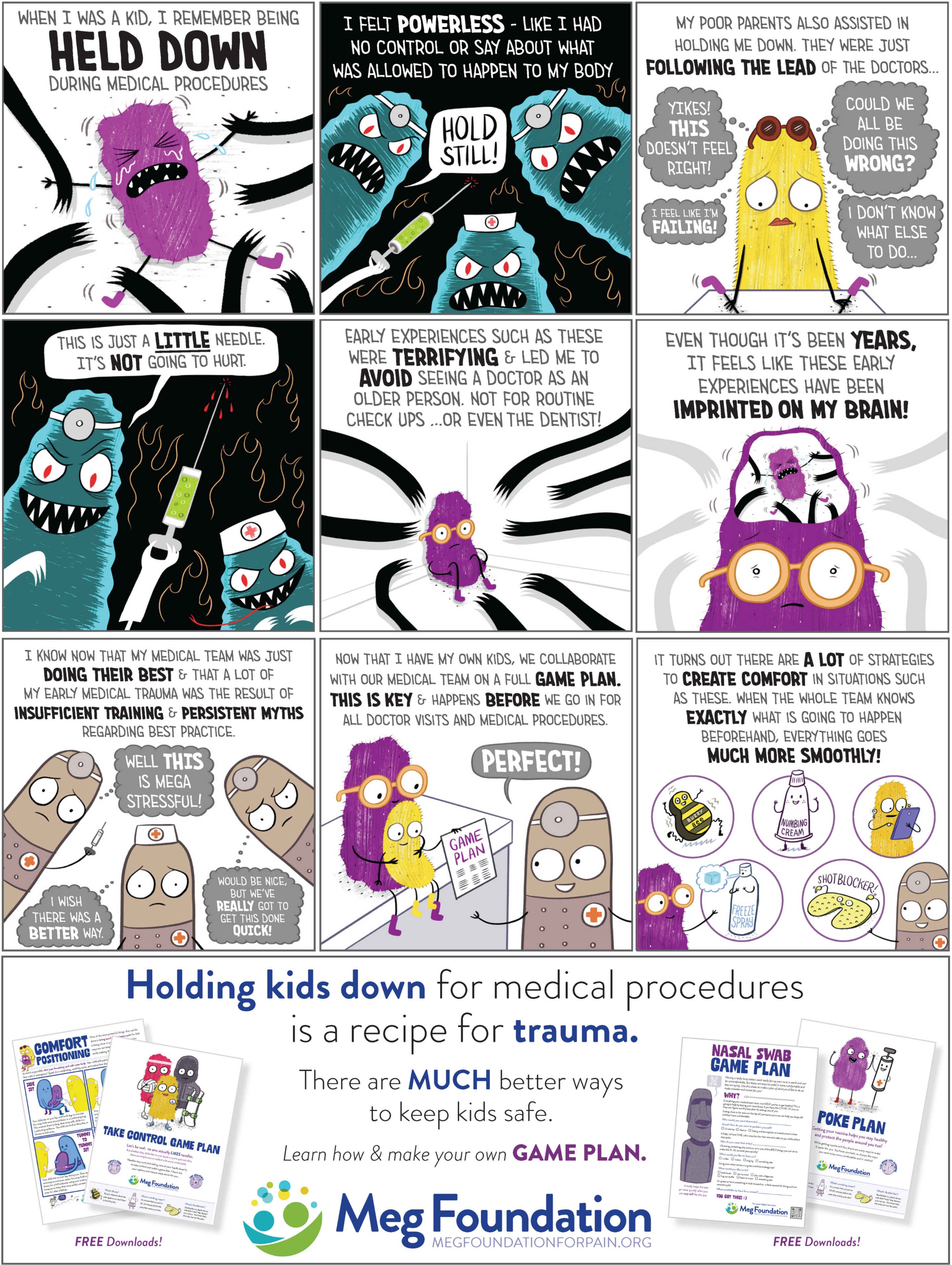
At The Meg Foundation, we’re always striving to foster understanding and empathy in everything we do and create. Today, we’re excited to share something unique—a comic that explores an adult recalling an early childhood memory about getting a shot at the doctor’s office. In this heartfelt portrayal (which reflects the experience of so many) a child’s fears manifest as imagined monsters. This depiction represents the intensity of fear, and feelings of powerlessness, they experience.
Clearly, we do not believe healthcare workers are monsters. In fact, we believe in their dedication, compassion, and commitment to healing. And we hope to share point-of-view comics that depict the perspectives of healthcare workers, too!
Please read our full statement to gain insight into how these comics reflect our core values, beliefs, and mission, while demonstrating our steadfast support for all the communities and individuals we serve—kids, parents, and healthcare providers alike.
So, what can we do instead?
There are effective and SAFE ways to keep kids still during procedures, so why does this still happen? Well, it certainly is NOT because medical providers are trying to hurt kids or that they don’t care. As with most things, it’s complicated, but we can break it down to these three:
- Lack of sufficient training
- The natural-if-unhelpful human tendency to do things “the way they’ve always been done.”
- Persistent myths
Let’s take a few minutes to dismantle some of the more dangerous of those myths:
Myth 1:
“We have to do this to keep them safe.”
Actually, no, you don’t. We can all agree that keeping kids safe during a needle stick or medical procedure is necessary, but holding them down (especially on their backs) is not keeping them safe. In fact, there is substantial evidence that holding kids down on their backs can be a recipe for medical trauma. It can spark future negative reactions of fear and panic at the thought of getting shots or even entering a doctor’s office or medical setting.
What they are actually referring to is keeping kids still enough to safely put the needle into their skin. That is important, but there are better ways than holding them down. More on that later.
Myth 2:
“I’ve been doing this for years. Holding them down is not a big deal – they probably won’t even remember it.”
I can tell you that I’m 47 years old and remember it like it was yesterday. I was four years old and being held down by four nurses for a blood draw as I screamed hysterically for my mother, who was waiting helplessly in the waiting room. My mom remembers the horror of sitting there listening to my terrified screams, unable to protect me. I can still picture the Muppets poster on the wall, and I remember that exact shade of blue of the nurse’s scrubs. Now, as an adult and expert that has treated medical trauma for years, I can assure you they will remember it.
Do you want to test the theory? Ask your friends about their earliest medical memory. You’ll hear stories of fear and panic and running out of exam rooms, usually followed by something like “I still hate shots…” or even worse (but unfortunately common), ”…and that’s why I don’t go to the doctor.” So not only do kids remember, they very often carry that memory and fear with them to future doctor visits and often into adulthood.
Myth 3:
“You can’t breastfeed during a needle poke…the baby can choke on your milk. They will learn to associate you with pain.”
Nope, not a thing. Babies are effective machines designed for eating, and there is no evidence that they will choke. And there is zero evidence that a 20-second procedure has the power to redefine your child’s attachment to you. It’s honestly a ridiculous idea.
On the contrary, the natural sugars in the milk, the primal soothing of the sucking motion, and the comfort of the mom’s warmth and skin are brilliant pain management tools. It actually biologically changes the ways pain is processed in the body. This a great video talking about babies under six months, and this one for over six months. Even if babies cry during a poke, they are quickly soothed by caregivers’ safe and comforting presence.
For babies not breastfeeding, the soothing warmth of being cuddled and comforted by a trusted parent or caregiver is HUGE for managing the pain of the poke. Skin-to-skin is even better. Sugar water on a pacifier is also fantastic and is a well researched pain management strategy for little ones.
Myth 4:
“This is the only way to keep them safe.”
A solid NO for this one. There is another way to keep kids safe and still for a procedure and be comforted by a trusted adult. It’s often called Comfort Positioning, and research has demonstrated the benefit for kids, parents, and medical providers. It allows parents to hold and comfort their children at the same time. Importantly, it allows providers to do their job safely and usually more quickly.
We have a guide here that quickly allows you to find the position that can work for your child and your situation (different positions are better for different procedures).
The power of a trusted adult’s physical presence, warmth, and reassurance makes a massive difference. There is a huge difference between being held down against your will by strangers and sitting on a parent’s lap in a bear hug, with mom’s (or dad’s or whoever’s) arm “helping your arm and body keep still so we can get things done quickly and safely.” One is potentially traumatic. The other is being thoughtfully supported in getting through what can be a challenging experience.
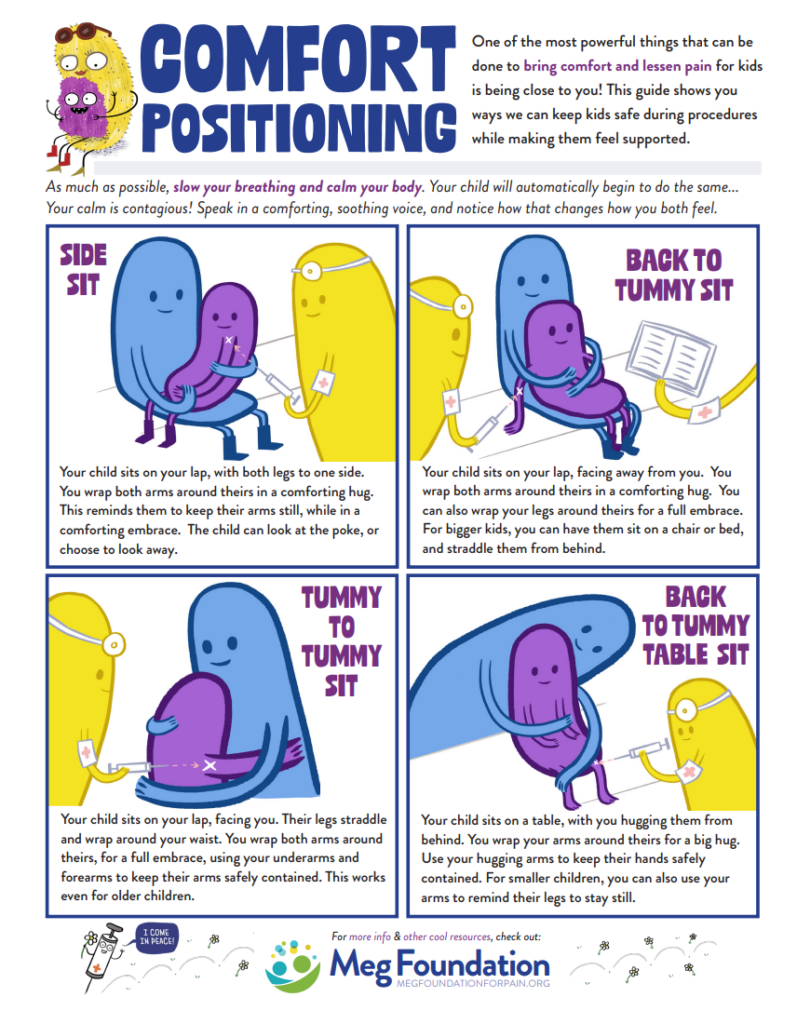
5 ways to maximize comfort positioning:
- Choice is power: Help kids feel more in control by having them choose as much as possible: which position do they prefer? Who sits with them? Which arm needs to keep still?
- Prep and practice: Look over positioning options and explain and practice what is going to happen at home or sometime BEFORE the procedure when there is less stress and pressure. It allows kids (and let’s be real…you too!) to work through their anxiety and helps kids and you feel better about knowing exactly how it is going to happen.
- Watch your language: Say things like “My arm is going to help your arm remember to keep still.” Rather than “I have to hold down your arm.” Praise positive efforts (“Nice job…you are doing great!”) and focus attention on positive sensations (“It feels so good to hug you…do you feel how warm it is against my chest?”) to draw focus away from harder ones.
- Calm yourself: Stress is contagious but so is calm. When you slow your own breathing and focus on calming yourself, your child will naturally and automatically do the same.
- Combine with other strategies: This is but one tool in the toolbox! When you combine these strategies with others (such as distraction, numbing cream, vibration, and breathing), you create an even bigger impact! Learn about every technique here in our parent’s guide to understanding pain.
It also needs to be said: this works for people of ALL ages. Parents and the medical world tend to shame older children, tweens, and teens as being “too old for this” when they express medical anxiety. PLEASE don’t do that. That shame is what sticks with people in very negative ways. Frankly, its what come up my psychologist couch even years later. We all need validation, empathy, and support, not shame. The powerful one two punch impact of touch and the presence of a trusted human to calm and soothe is something that thankfully we never outgrow.
Whether it’s a flu shot, vaccine, blood draw, stitches, or just blood pressure, comfort positioning can make this easier and better for you, your child, AND the healthcare provider. Everybody wins.
A little heads up: you may have to push for this and against advice from healthcare professionals to hold down your child.
While I know advocating in a medical setting can seem hard or intimidating, remember that everyone has a common goal: to make this experience as good as possible for your child. Use your voice, trust the science, and please don’t let them hold down your kid. We have your back!
— Our Commitment —
Shaping the future of pain care, one diverse perspective at a time
What did you think of our new comic?!
Here at Team Meg, we recognize the significance of releasing this comic—our unique and novel approach to sharing stories from multiple perspectives in an effort to foster empathy and drive transformation in pain care. But exploring one perspective at a time will likely generate all sorts of reactions, including some that are unintended or unforeseen. For this reason, we are providing additional explanation and context now. We want to ensure our intentions and the broader impact of this effort are clearly understood, encouraging respectful dialogue and meaningful engagement.
First, we believe it is important to be brave when having hard conversations.
Big change doesn’t happen in the absence of curiosity, openness, empathy, and honest dialogue. We hope you’ll join us in striving for all these things.
Second, we believe in the power of storytelling and seeing the world from someone else’s point of view.
By sharing different perspectives, we create the opportunity for connection which can lead to a world-changing shift in how we all think about kids and pain.
This comic, in particular, focuses on the perspective of a child. This doesn’t mean we don’t value the perspective of providers, caregivers, or others. In fact, our goal is to share all perspectives so we can create a greater sense of understanding. This also highlights the fact that we all share a common goal: eliminating unnecessary pain and suffering.
Third, we believe the gap between medical research and the practice of good pain management is the byproduct of a very imperfect medical system, not the healthcare providers working in it.
We love healthcare providers! And we don’t want our highlighting of where systems fail patients, families, and providers themselves to be viewed as placing blame on any one individual. There are no villains here.
When the intent of an intervention (like a medical procedure) and unintended outcomes (like medical trauma) are so incredibly far apart, humans have a hard time seeing hard truths. This is natural and the reason why it is so important, but still hard, to be brave and curious.
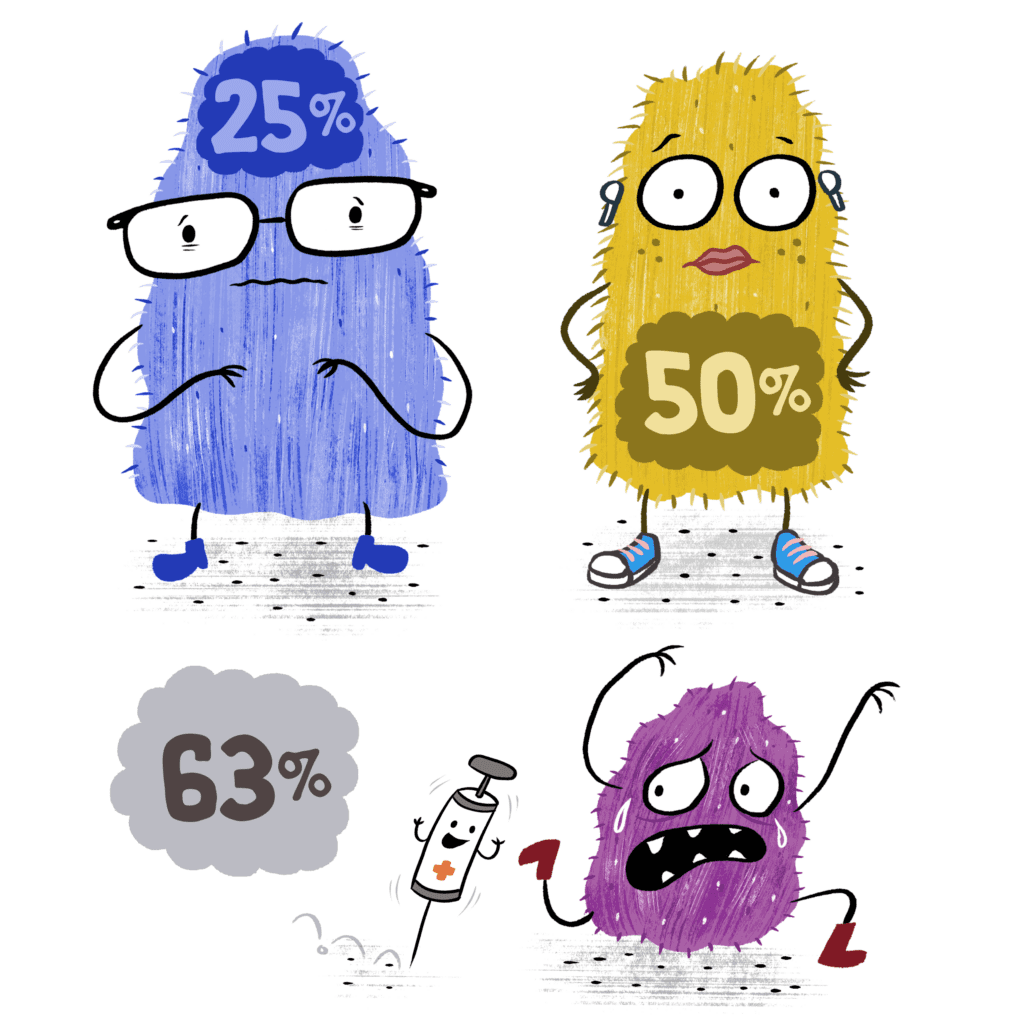
The child’s perspective of needle fear and anxiety, portrayed in this comic, is shared by many. We hear it when asking about pain experiences, we read it in the comment sections of procedural pain videos, and we see it in data that tells us that 63% of kids, 50% of teens, and 25% of adults have significant needle fear. This fear ends up impacting people’s medical decisions throughout their lives.
The good news: solutions exist that can make all this better.
And the Meg Foundation is here to help! Empowering people with the pain management strategies, skills, and support they need to prevent and reduce pain is what we know, do, and love. So we tell this story not to place blame, but to encourage dialogue, inspire action, and create change.
These stories, even the ones that are difficult to share, are important and deserve being told. Your story is important, too, which is why we want to hear it! Please share your experiences and perspective with us. Let’s keep this conversation going so we can take more informed steps together.
We are always here, we are always listening, and we will always use our voice and platform for good.
With gratitude and humility,
Team Meg

Are you a healthcare provider?
Check out this resource to improve your practice! This eBook guide outlines the what, the why, and the HOW of good pain procedural management for medical providers.
You May Also Be Interested In
Downloads
Comfort Positioning Guide
Learn comfort positions that allow you to calm and comfort your child while keeping them safe!

Article
American Academy of Pediatrics: Taking Fear and Pain Out of Needles-For Your Child and You
Great article with practical tips from HealthChildren.org, the website of the American Academy of Pediatrics.

Digital Tool
Pain Champions Guide for Parents
Learn all you need to know about how to manage needle pain and anxiety through this interactive tech tool.

Downloads
Creating Comfort for Kids Printable Poster
Let our monsters teach kids and families how to prevent pain and anxiety during needle pokes!

About the Author
Dr. Jody Thomas is a licensed clinical psychologist, and specialist in pediatric medical illness and trauma. A well-known expert in pediatric pain who teaches internationally on the subject, she is also a founder and the former Clinical Director of the Packard Pediatric Pain Rehabilitation Center at Stanford, and a former Assistant Professor at the Stanford University School of Medicine. Though she now lives in Denver, CO, she still serves as Adjunct Faculty for Stanford, providing supervision and teaching. As a consultant for the Lucile Packard Children’s Hospital at Stanford, she directs projects on the integration and innovation of pain management using tech-based intervention. Her passion for bringing together the power of medical science, technology and design to transform the way we think about kids and pain led her to her current focus but it’s her role as a mom of two that solidified her path in creating the Meg Foundation.