Pain Management for Trans and Gender Diverse Youth
We’re all about supporting children and families with resources that help them be more comfortable and less anxious during medical procedures. For trans and gender-diverse youth, the word “empowerment” is a critical part of their medical vocabulary.

Jessica Bernacki, PhD
Kids (3-11) Tweens & Teens (12+) Needle Pokes Provider Acute Pain Chronic Pain Procedural Pain English Pain Management
Share this:
“It’s all about empowerment and self-efficacy,” says Dr. Jess Bernacki, Meg Foundation Advisory Board Member and clinical psychologist specializing in affirmative therapy for transgender and gender diverse (TGD) youth and adults. “It’s critical that these kids feel more in control and involved in how they’re being referred to, how they’re feeling in their body, what’s working, and what’s not working for them. Pain management is just one more way to foster that self-efficacy and help them feel empowered.”
For TGD youth, early puberty marks one decision point for potential intervention. “This is when we start the conversation about whether the adolescent is prepared to go through the puberty that their body is programmed to do,” explains Dr. Bernacki. “If they’re not, there are medical interventions we can pursue that will pause puberty.”
Pausing puberty can be accomplished through injectable blockers or implants. Both injectables and implants are temporary and require lab work before, during, and after to check hormone levels and maintain the health of the patient.
In short: a lot of potential needle pokes and discomfort.
Now, the good news! TGD youth can use resources like the ones provided by Meg Foundation to manage their pain and feel more prepared for procedures. Here are a couple of ideas:

Anxiety & pain around needle pokes
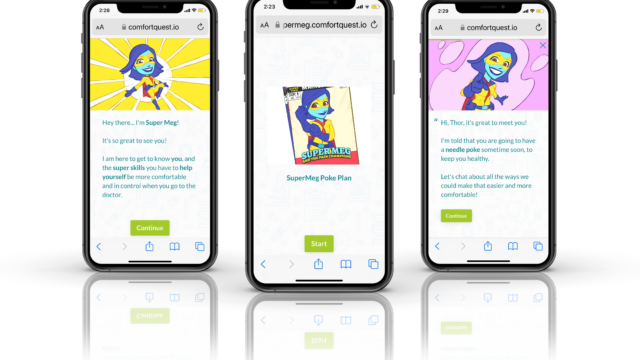
We’ve written a lot about expert, research-backed strategies to make needle pokes more comfortable. Now, we also have TWO digital tools that teach kids strategies and help them create a personalized plan. For younger kids, check out our cool interactive tech SuperMeg, which leads kids through choosing the strategies that they want to work for them (and sends that plan to their parent). Teens and tweens can check out the Take Control web app, which introduces all the strategies, breaks down the why and the how, and sends them their own personalized plan.
Quick guide to topical anesthetics, aka numbing cream
Using numbing cream is one of the top best-practice recommendations for medical procedures. Not only does numbing cream reduce physical pain, but it increases patient confidence and reduces anxiety. Check out our guide and be sure to discuss what options might work best for your procedure with your medical provider. This video breaks it down for you too.
Vibration: the secret weapon that REALLY works
So it turns out that pain actually happens in your brain! By using vibration, we can create a traffic jam of signals on your nervous system that blocks the pain signal from ever reaching your brain…and that can feel a LOT more comfortable. This video explains more!
Self-regulation with ImaginAction
Stanford Children’s Health put out this great self-regulation tool that can help kids (and adults) feel more in control of their emotions, thoughts, and behaviors. ImaginAction can help users feel less anxious, feel more okay with uncertainty, manage pain, and more. Check out the great explainer video on their homepage to learn more!
Want to learn more about how pain actually works? Check out this cool handout the for a quick and easy breakdown that opens us all sorts of possibilities for feeling more comfortable and in control.
Resources just for tweens and teens
Meg Foundation’s Tweens and Teens section has a whole bunch of other expert-vetted resources for kids 12 and up. Don’t see a resource or have a question? Don’t hesitate to reach out at info@megfoundationforpain.org.
We wish it were standard clinical practice for these techniques to accompany any medical procedure, but until they are, we’re here to help you advocate for them.
One final note– it’s important for clinicians to remember that it’s INCREDIBLE common for people to get really anxious about needle pokes and procedures. Sixty-three percent of kids, 50% of teenagers, and 25% of adults have this issue. So a gender diverse kiddo have anxiety about medical procedures very likely isn’t about questioning their choices…it’s about really not liking needles! As Dr. Bernacki points out, “A youth can be experiencing anxiety about a procedure AND be experiencing gender dysphoria. Neither takes away from the experience of another. Engaging a youth in conversation about those feelings will help distill that.” As always, it’s important to listen, engage, and be open and accepting.
At the Meg Foundation, we are all about giving you vetted resources you can trust, and we want to connect you with other nonprofits and advocacy organizations that can do that too. Here are three fantastic nonprofits doing great work in the LGBTQia community and have incredible resources available:
InReach is a trans-led tech nonprofit increasing resource access for the diverse LGBTQ+ community. The free InReach App is the world’s first tech platform matching LGBTQ+ people facing persecution or discrimination with safe, verified resources.
OkaySo uses a free mobile app to connect LGBTQ+ young people who need help to experts who provide personalized support and information. It doesn’t matter who a young person is, where they are, or what time it is, OkaySo’s experts will be there.
Worthy Mentoring is a tech nonprofit that empowers the LGBTQ+ community in coming out and being out. Our free mobile app allows mentees to connect with verified, trained, and screened mentors for support in understanding, accepting, and loving your LGBTQ+ identity.
You May Also Be Interested In
Digital Tool
SuperMeg Poke Planner
Have no fear, SuperMeg is here! This interactive tech helps your child create a plan for being more calm and comfortable during needle pokes.

Digital Tool
Take Control Mobile App for Teens
We want teenagers to feel powerful and in control when it comes to their bodies and their health care! This tech tool (which works best on phones) helps them learn the strategies and create a plan to feel more comfortable at their vaccine, blood test, or other medical procedure.

Downloads
Printable Take Control Poke Plan for Teens
We all do better with a plan! Use this to help teens create one of their very own before their next poke.

About the Author
Dr. Jessica Bernacki is a licensed clinical psychologist in the Department of Medicine at the UCLA Medicine-Pediatrics Comprehensive Care Center and on the Pediatric Psychiatry Consultation-Liaison Service at the UCLA Medical Center, Santa Monica. Her clinical, teaching, and research interests focus on the delivery of evidence-based behavioral health services in the primary care setting and coping with pediatric medical illness. It is from her experiences working in pediatric inpatient and outpatient care at UCLA and Lucile Packard Children’s Hospital at Stanford, as well as having her own two children, that have motivated her to help improve the experience of youth receiving medical interventions.